What Are 6 Ultrasound Uses?
Category
Blog
Date
February 25, 2023
Source
Exo

Over the decades since its first emergence, the ultrasound machine has seen a lot of evolution. Douglass Howry’s 1958 Pan Scanner was a crucial predecessor to the modern portable ultrasound machine. Using a modified dental chair, a saline-filled pan, and a rotating ultrasonic transducer, Howry’s Pan Scanner performed some of the first clinical scans of the human abdominal area.
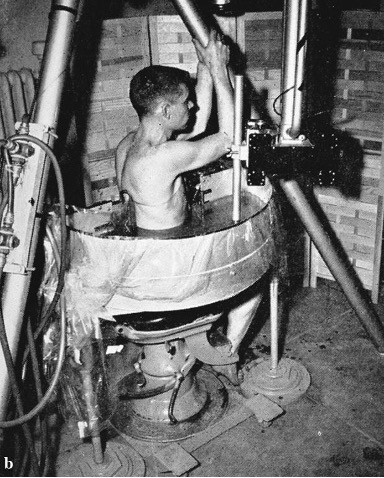
This clever contraption was one in a series of developments by Howry’s team. Some initial models required full submersion of the subject in a livestock watering tank with a lead weight wrapped around their abdomen to prevent floating. These machines were successful at ultrasound imaging, but Howry’s team recognized they presented challenges in practice. Can you imagine asking patients to weigh themselves down and climb into a saline-filled cattle trough, all for a basic ultrasound exam?
Thankfully, cattle trough setups are a thing of the past. Present-day ultrasound machinery is much more elegant and mission-critical in comparison. With such advancements comes a higher demand, and market researchers anticipate the ultrasound device market will see a compound annual growth rate of 4.5% over the next decade.
Why have ultrasound machines become a clinician’s preferred sidekick? While commonly associated with procedural prenatal scans and health screenings, ultrasound machines are also powerful diagnostic tools in the emergency room. Recent studies have demonstrated the advantages of ultrasound machines in emergency departments, including more cost-effective care overall. Ultimately, that real-time look inside a patient is invaluable when making life-altering treatment decisions in mere minutes.
Whether you’re new to ultrasound or an expert looking to modernize your facility’s ultrasound practice, this blog will review the basics of ultrasound machines, their portability and uses in modern medicine, and how to improve point-of-care ultrasound workflow to accelerate improved standards of care at your healthcare facility.
What Are the Components of an Ultrasound Test?
An ultrasound test involves capturing images of internal body structures using high-frequency sound waves above the human hearing range. The various ultrasound machine parts and functions that allow clinicians to complete these tests include:
- Pulse Transmitter: The transmitter produces short bursts of sound waves through a transducer.
- Transducer: This is the handheld probe placed on and moved over a patient.
- Control Unit: The operator will have a control unit to modify the amplitude, duration, and frequency of emitted pulses. They can also take measurements directly on the imagery and input other data or notes.
- Central Processing Unit (CPU): A CPU is necessary to digitally process sound waves into imagery.
- Display System: Most ultrasound machines have a real-time display showing the area beneath the transducer.
- Workflow: Exam automation has sped up and standardized the modern-day ultrasound exam process. A high-quality ultrasound workflow will provide this support while seamlessly connecting clinicians, administrators, and patients to the records.
- Device or Cloud Storage: All scans should be recorded and saved to an on-premise database or cloud storage.
How Does an Ultrasound Machine Work?
Ultrasound machine technology has evolved greatly, thanks to the work of multiple researchers studying the application of sound in medicine. In broad strokes, an ultrasound machine works as follows:
- The pulse transmitter produces sound waves through the transducer (aka the “probe”).
- The sound waves travel until they hit various body tissues, causing the sound waves to bounce back at different rates.
- These returning sound waves, or “echoes,” are received by the transducer.
- The transducer sends the data to a CPU that translates the echoes into an image.
The tissue’s density will control how quickly the sound waves return to the transducer. If there is nothing for the sound waves to bounce off of, the resulting image is black. For example, the amniotic fluid surrounding a fetus appears black in a sonogram because sound waves travel through liquid. When the sound waves encounter a fetus, the returning echoes result in white and gray outlines of tiny human features.
What Are the Types of Point-of-Care Ultrasound Machines?
Regarding the types of ultrasound machines that prize portability for increased attention to patients at the bedside, there are three main varieties available for purchase:
- Cart-Based: A cart-based machine is usually the first image that comes to mind for most when they hear “ultrasound.” These large systems are generally on wheels and stay within their designated facility department (like a specific ward or radiology department).
- Portable: Although bulky, these more portable ultrasound machines allow doctors to carry the machines to the patient’s bedside, whether in the hospital, the patient’s home, or a remote location. The machines in this category today resemble laptops with wired (and some even wireless) transducer attachments.
- Handheld/Pocket-Sized: This category of ultrasound machine applies to pocket-sized, battery-powered devices, which started popping up in the more recent decades. Nowadays, clinicians can run ultrasound exams from smartphone and tablet apps connected to handheld (sometimes wireless) transducers—also called a “device-based” ultrasound exam.
What Are 6 Common Uses of Ultrasound?
The uses of ultrasound in medicine are ever-expanding, especially as portable devices become more advanced and widespread. Here are some ways clinicians use ultrasound technology to improve patient care.
1. Trauma
Unintentional injury is one of the leading causes of death among people younger than 45 years old, according to the Centers for Disease Control and Prevention (CDC). Falling, drowning, and motor vehicle accidents are some of the top causes of these trauma-related deaths. With the imminent risk of hypovolemic shock or intraperitoneal bleeding, clinicians need a quick, non-invasive, and accurate way to assess injuries.
An ultrasound exam can offer just that. Certain ultrasound protocols, like the Focused Assessment with Sonography in Trauma (FAST), have allowed providers to complete these exams in less than five minutes. The speed of these ultrasound exams gives back valuable time to patients with life-threatening injuries.
Does the speed decrease the accuracy of readings in these high-stress situations? Not at all—ultrasound use has proven to decrease time to surgical intervention, rates of CT scans and diagnostic peritoneal lavage, and a patient’s length of stay.
2. Pregnancy and Obstetrics
Ultrasound machines have significantly reduced fetal and maternal mortality rates. One recent study found that ultrasound exams reduced fetal deaths by 20% and post-term delivery deaths by 50%. Another study of 460 pregnant people concluded that using handheld ultrasound machines could have averted 6.3% of maternal deaths and 14.6% of neonatal deaths at the time of delivery.
Clinicians use ultrasound machines to evaluate and look for a variety of conditions in the birthing parent and the fetus, such as:
- Fetal viability
- The number of fetuses (and evaluating chorionicity and amnionicity, if necessary)
- Location of the gestational sac
- Gestational age
- Chromosomal abnormalities
- Any anomalies, like fetal heart defects or ectopic pregnancy
3. Abdominal Assessment
What can an abdominal ultrasound detect? An easier question to answer would be—what can’t an abdominal ultrasound detect? Sound waves do not travel well through bones or air, so affected areas concealed by bone or gas may require an X-ray, CT, or MRI scan. However, even with these limitations, ultrasound machines can still detect numerous medical conditions throughout the abdomen, like:
- Hydronephrosis caused by renal blockage- Renal colic (pain caused by kidney stones) has an estimated prevalence of affecting one in every 11 people. An ultrasound exam helps clinicians determine the severity of hydronephrosis. Lack of hydronephrosis reduces the likelihood of a larger stone, which is an essential observation during risk stratification.
- Appendicitis: Ultrasound is usually the first line of diagnostic defense when it comes to suspected appendicitis, especially for pediatric patients so they can avoid radiation with CT scans. One study found that routine ultrasonography for appendicitis assessment reduces negative appendectomy rates from 22.5% to 4.7%.
- Cholecystitis and Gallstones: Clinicians can identify thickened gallbladder walls, pericolic fluid, gallbladder sludge and stones, and bile duct stones with an abdominal ultrasound. In fact, one scientific review determined that ultrasonography was 90% to 95% accurate in detecting gallstones because of all these quickly identifiable signs.
- Bowel Obstruction and Perforation: Can an abdominal ultrasound detect bowel problems? Although MRI and CT scans are more accurate for bowel imaging, ultrasonography is still quite effective. Unlike MRI and CT scans, clinicians can perform ultrasound exams at the patient’s bedside, resulting in quicker diagnosis and less stress and movement for the patient. It’s also a relatively simple exam for new residents—one study demonstrated emergency medicine residents with limited small bowel obstruction (SBO) ultrasound experience could still perform SBO exams with high accuracy.
4. Procedural Navigation
Placing needles and tubes into a patient presents a myriad of challenges. Thankfully, an ultrasound’s real-time visualization makes this kind of anatomical navigation much more manageable. For example, ultrasonography has proven to be the fastest method of confirming correct tube placement when performing endotracheal intubation compared to capnography and chest auscultation.
Ultrasound guidance also comes in handy for lumbar puncture (LP) procedures. These exams require transverse and longitudinal scanning to map the lumbar spine for optimal needle insertion. Randomized trials have revealed that using an ultrasound machine during an LP reduces the number of traumatic tap attempts and improves LP success rates.
Clinicians also commonly utilize ultrasound machines for:
- Nasogastric tube placement
- Peripheral nerve blocks
- Establishing venous access centrally and peripherally
5. Vascular Assessment
Observing a patient’s blood flow through arteries and veins can reveal numerous medical conditions. A Doppler ultrasound is typically used for this assessment, as clinicians can use these to calculate the speed of blood flow. It works by measuring the Doppler effect, which occurs when a sound wave source is moving relative to an observer, causing a change in the wave's frequency and wavelength. As blood cells move closer and further away from the ultrasound probe, their reflected sound waves change frequency, allowing clinicians to measure the speed of blood flow.
A common condition easily identified with this ultrasound technology is deep venous thrombosis (DVT). If detected too late, DVT can lead to superior vena cava syndrome, pulmonary embolism, and other potentially deadly complications. Studies show that only 23% to 50% of patients present with classic symptoms of DVT, which makes an ultrasound extra helpful when patients aren’t showing these symptoms. By identifying DVT early on with a bedside ultrasound exam, clinicians and their patients can look forward to:
- Avoiding unnecessary testing, like the d-dimer test (which has a high rate of false positives)
- Avoiding formal ultrasonography, which can take an extra hour to perform
- Decreasing emergency room length of stay by approximately two hours
6. Cardiac Assessment
The use of ultrasound for cardiac assessments has become invaluable. For example, consider abdominal aortic aneurysm (AAA), which has a high mortality rate of 50% to 95% once ruptured. The trio of abdominal pain, hypotension, and a pulsating abdominal mass usually point to an AAA, but multiple studies show that less than 25% of patients will present with these obvious indicators. Even worse, around 30% of AAAs are misdiagnosed on initial presentation after rupture. However, with bedside ultrasound use, mortality rates can decrease between 20% to 60%.
Even handheld ultrasound devices have made great strides in providing useful insight into the following heart conditions:
- Pericardial effusion
- Pericardial tamponade
- Significant valvular stenosis and regurgitation
- Decreased ejection fraction
- Ventricular dilatation or hypertrophy
What Are the Uses of Ultrasound Workflows?
Beyond ultrasound machine uses in clinical settings, providers should also consider the backend workflow of ultrasound imaging. This workflow can quickly get messy, with clinicians juggling bedside care, documentation, quality assurance, and resident training. And as POCUS and device-based ultrasounds become more common, tracking imaging for record-keeping, billing, and liability purposes has become more complex.
Instead of cobbling together multiple systems for a makeshift workflow, consider using Exo Works™. The Exo Works platform will securely take you from scanning to completed documentation in mere seconds. This app provides:
- Modules for clinical and educational use
- Questions and worksheets to guide users through an exam
- Built-in billing information with CPT codes to support reimbursement
Exo Works also simplifies quality assurance (QA) by making ultrasound exams available instantly for review or collaboration—from work or from home. Reviewing clinicians can take advantage of markup tools and image tagging to streamline the entire QA process. The app is so user-friendly that clinicians can power through their workflows without having to bug IT.
Don’t let complicated or lacking workflows undermine your POCUS processes and reimbursement. With Exo Works, ultrasound management and monitoring become much easier, saving clinicians valuable time and increasing the quality of patient care. See how it can make your work life better here.